Our research questions
Our primary research question is, ‘how do we develop resilience capacities to ensure responsive, effective, inclusive, gender-equitable and sustainable health systems in fragile and shock-prone settings?’
Within that there are a number of other questions which we are addressing:
- How can coordination between overlapping national health systems and providers be improved?
- How can service delivery change to increase uptake by particularly vulnerable groups?
- What are the politics of intervention implementation in fragile settings and how do actors and arising powers influence services?
- How can we use evidence to strengthen health systems and routine and emergency service planning in decentralised contexts?
- What metrics and processes are appropriate for appraising health system resilience?
- What are the most effective tools to improve monitoring and accountability?
- How can we build more inclusive and gender transformative models of care?
The resilience framework
This short animation explains what we mean by ‘resilience’ and the framework we are using to study its elements.
There’s more on the resilience framework outlined here
Our approach to resilience is informed by work done by the team on health system resilience (Ager et al. 2015), organisational resilience (Alameddine et al. 2018) and individual resilience (Witter et al. 2017), which empirically modelled the feedback loops through which systems can manage shocks. ReBUILD for Resilience will take this work forward, further examining the capacities which underlie resilience and how these can be built and maintained. At its core, resilience concerns a system’s ability to flex in response to shocks and stresses. However, we recognise that systems perform at different levels, which is why our research will also focus on responsive, effective, inclusive, gender-equitable and sustainable systems.
Theory of change
How will our research improve life for the 1.8 billion people living in fragile contexts? Our theory of change outlines the process.
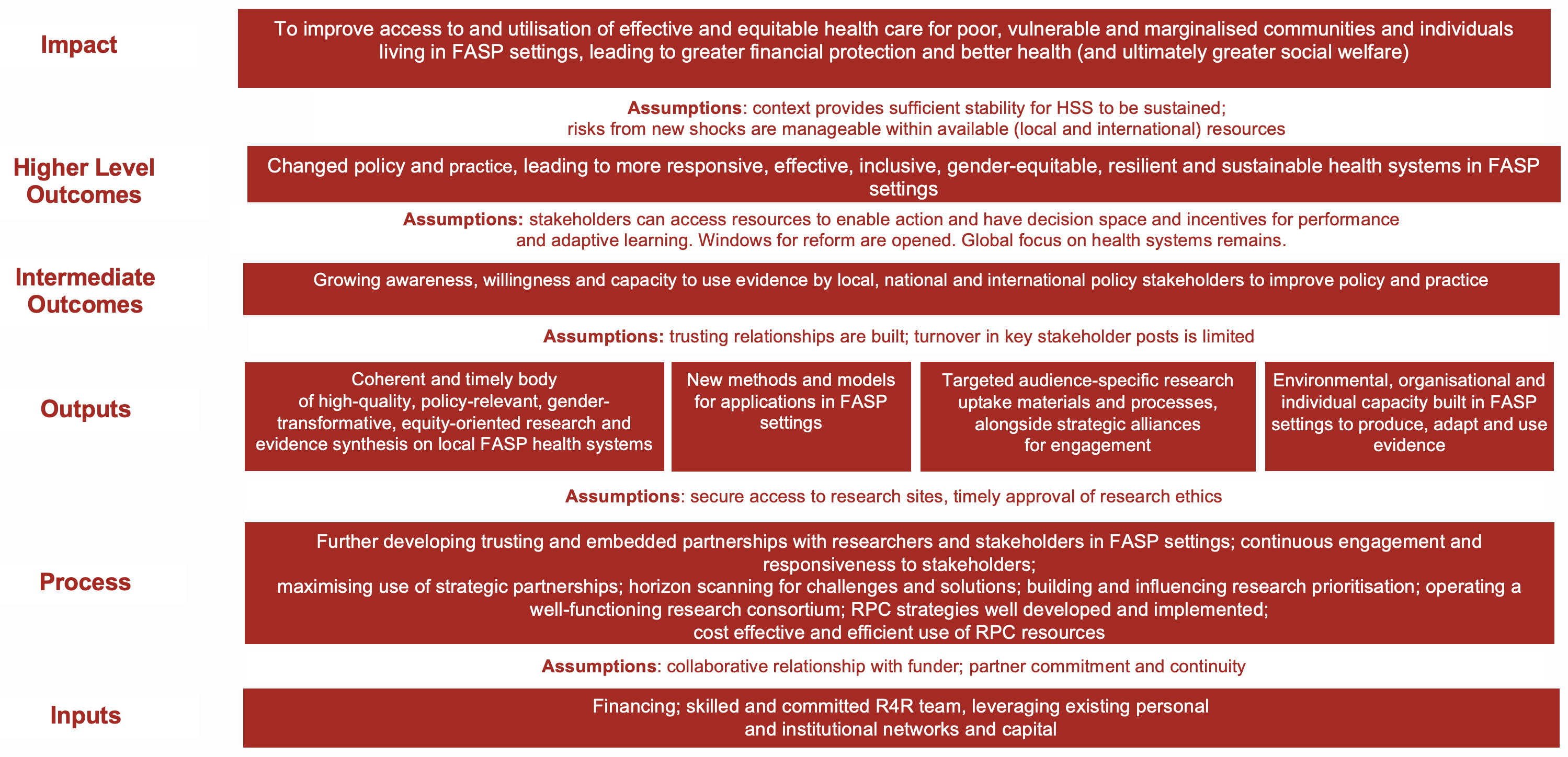
The diagram shows how inputs and processes will lead to outputs, such as high-quality research, which will in turn contribute to growing awareness, willingness and capacity to use evidence by local, national and international policy stakeholders. This will then contribute to changed policy and practice, leading to stronger and more resilient health systems, and ultimately improve access to and use of effective and equitable health care by people living in fragile and shock-prone settings.
Our methods
The main approaches to be used, clustered by function, are:
Exploratory and developmental research: problem diagnostics, situation analysis, social network analysis, social connections analysis, life histories, participatory methods such as Photo Voice, feasibility assessment of pilots, policy analysis, expert and community consultation, capacity assessments, appreciative enquiry/positive deviance, political economy analysis, stakeholder mapping, discrete choice experiments
Explanatory: case studies, using mixed methods (often combining observation, interviews, focus groups, document analysis and surveys), prospective studies using quasi-experimental designs, analysis of routine health system data, re-analysis of existing data sets, cross-country comparative analysis, systems dynamic modelling
Evaluative research: impact evaluation, theory-based methods (including realist), contribution analysis, most significant change methods, implementation and process evaluation, participatory action research, outcome mapping, value for money analysis
Methodological and reflective learning: development of conceptual frameworks, improved metrics (eg for resilience and HSS), toolkits for research and engagement, intersectional approaches and analyses, assessment of effectiveness of our research, capacity-strengthening and research uptake strategies
Evidence synthesis: rapid reviews, scoping reviews, participatory reviews, systematic reviews
In all cases, we will start with a review of existing evidence, and research will draw on available data, while also attempting to strengthen these data in future. We will prioritise evidence and learning which can be generated from existing data, such as re-analysis of data sets, building on the wider resources of partners and associates and the flexible funding modalities planned.
As we are concerned with understanding what, why and how interventions (such as policies, guidelines, programmes, technologies or practices) work (or not) in ‘real world’ settings and testing approaches to improve them, we will mainly use implementation and embedded research approaches.
Throughout our work we will remain focused on equity, gender, disability, justice and social inclusion. We will provide on-going training and mentorship to staff and build on our gender and health system work in ReBUILD.
Our outcomes
ReBUILD for Resilience will deliver high-quality, practical, multidisciplinary, operationally-relevant and scalable health system research in fragile and shock-prone settings.
As well as academic papers and briefing notes, we will produce a range of high-quality and demand-led outputs such as ‘how to’ guides for local decision makers, client engagement tools, methods toolkits and cross-country analyses. This learning will be disseminated through a comprehensive research uptake strategy.
You will find these outputs in the resources section.
Together these will contribute to strengthening resilience and building stronger systems for health across multiple levels (including at community level) and sectors (public, private, informal and mixes of these).